Abstract
Diarrheal disease is a common cause of pediatric morbidity of varied etiologies, with stool culture being a tool for bacterial diagnostic identification.
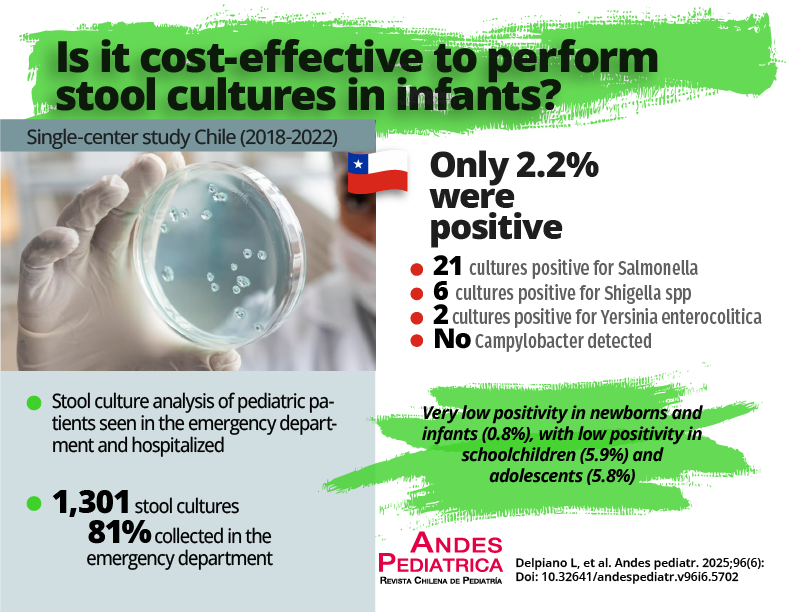
Objective: To evaluate stool culture positivity in pediatrics according to age, request source, relationship with hospitalization length, and costs.
Patients and Method: A 5-year review (2018 to 2022) evaluated the positivity of stool cultures collected from pediatric patients in the Pediatric Emergency Department and inpatient units of a public hospital, as well as the costs associated with the test.
Results: 1,301 stool cultures were included, 81% of them collected in the Emergency Department and 37.3% in hospitalized infants. The overall positivity rate was 2.2%, with 29 positive results, and a predominance of Salmonella spp. (n = 21) and Shigella spp. (n = 6). Campylobacter was not detected using Hucker staining. Positivity was low in infants, whereas schoolchildren and adolescents showed significantly higher positivity rates (p = 0.001). Among hospitalized patients, there was a significant difference in positivity when the test was requested within 72 hours from admission. It is noteworthy that in the Emergency Department, most of the patients with positive stool cultures were not hospitalized.
Conclusion: The test yield was low, especially in infants, which calls into question the actual usefulness of performing stool cultures in all patients with gastroenteritis, given its low clinical impact and increased costs. It is also reiterated that requesting this test in hospitalized patients after 72 hours from admission should be avoided, and that specific methods for Campylobacter detection should be routinely incorporated.

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright (c) 2025 Luis Delpiano M., José Manuel Campos R ., Felipe Castillo C. , Pablo Correa R., Catalina Le Roy O.