Abstract
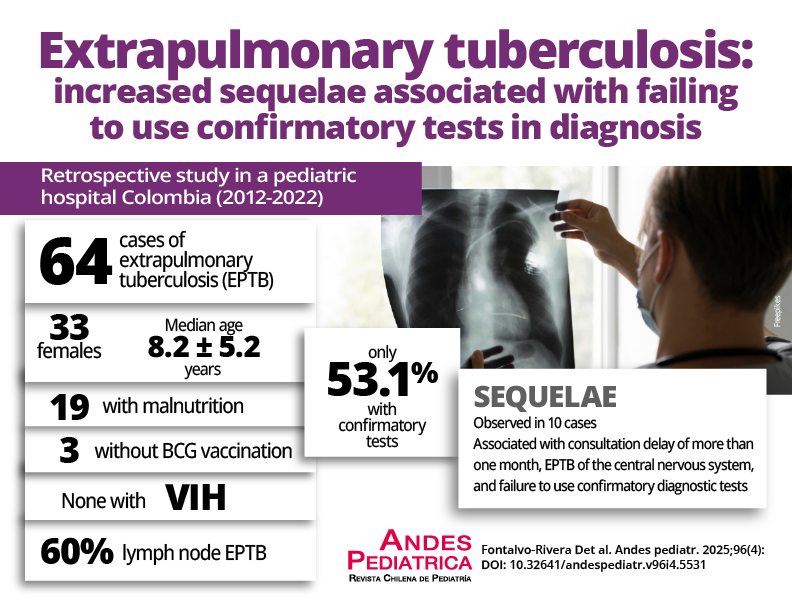
The diagnosis of extrapulmonary tuberculosis (EPTB) in children is challenging due to the variable and nonspecific manifestations and the low rate of M. tuberculosis isolations which delayed diagnosis, leading to an increase in cases with unfavorable outcomes.
Objective: To describe the use of traditional and confirmatory diagnostic methods for EPTB at the point of care (POC) in pediatric patients at a referral hospital.
Patients and Method: Retrospective study in both male and female patients aged 0-17 years hospitalized from January 2012 to January 2022 in a pediatric referral hospital in Cartagena de Indias, Colombia. Sociodemographic, clinical, and microbiological variables were analyzed. A descriptive analysis of the variables according to their nature was performed using frequency distribution, confidence intervals, and measures of central tendency with statistical significance of p≤0.005.
Results: Sixty-four cases were identified, with a mean age of 8.2±5.2 years and 51.6% were female. 30.2% (95% CI 19.2-43%) presented malnutrition, and 11.1% (95% CI 4.6-21.6%) were at risk of malnutrition. EPTB was found in the following areas: lymph node (60%), meningeal (7.8%), lymph node with peritoneal (7.8%), cutaneous, bone (vertebral), and peritoneal (6.3% each), and gastrointestinal and renal (3.1% each). Sequelae occurred more in cases when confirmatory tests were not used (60%) (p=0.0285). Confirmatory tests were used in 34 patients (53.1%), including solid medium culture in 29.7% of cases, of which 26.3% were positive. Molecular biology testing was used in 20.3% of cases, of which 53.6% were positive for M. tuberculosis. Among the factors that could have favored the development of sequelae were the time of consultation, the type of EPTB, and the use of confirmatory tests. In the latter case, they were more common in cases where confirmatory tests were not used (60%) (p=0.0285).
Conclusion: The wide range of clinical manifestations of EPTB can be confused with other pathologies that, combined with the paucibacillary condition, can delay timely diagnosis. The use of confirmatory tests at the POC and interdisciplinary management leading to a timely diagnosis and management would allow a decrease in undesirable outcomes in pediatric EPTB. Analytical studies are needed to infer this behavior.

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright (c) 2025 Revista Chilena de Pediatría