Abstract
The global prevalence of Periventricular Leukomalacia (PVL) has remained stable (~4%) in very low birth weight (VLBW) infants in the NEOCOSUR Neonatal Network for 16 years.
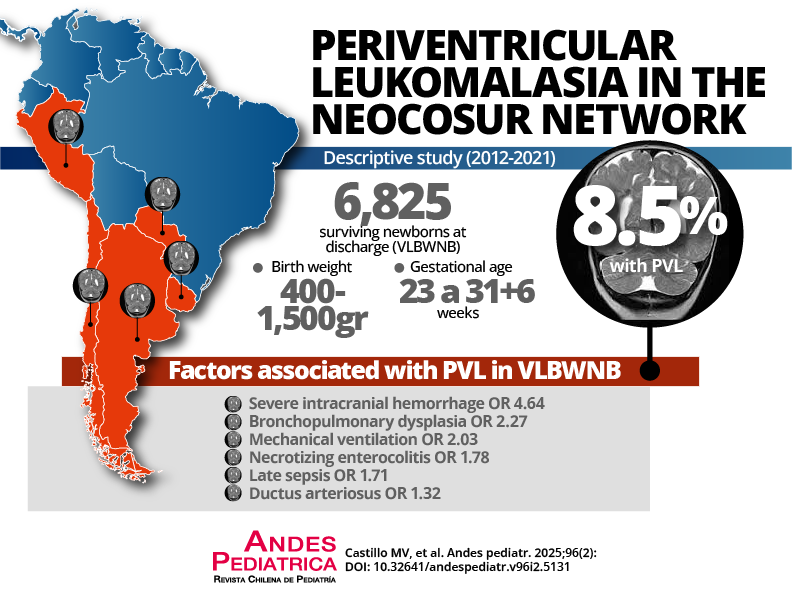
Objective: To determine the factors associated with the presence of PVL in surviving VLBW infants at discharge, its overall incidence, and gestational age (GA).
Patients and Method: Observational, multicenter, retrospective study with prospectively recorded data (period 2012 - 2021). Newborns with birth weight between 400 to 1500 g and 23 to 31+6 weeks of GA surviving at discharge were included. A bivariate analysis was performed using Pearson’s chi-square test to contrast the percentage of PVL for categorical variables and the student’s t-test to contrast averages for numerical variables. To explore the independent effect of each explanatory variable, a multivariate logistic regression analysis was performed.
Results: In 6,825 surviving VLBW newborns, the global incidence of PVL was 8.5%. Factors associated with increased likelihood of PVL were bronchopulmonary dysplasia (BPD) [OR 2.27; 95% CI 1.80-2.87], necrotizing enterocolitis (NEC) [OR 1.78; 95% CI 1.35-2.34], late-onset sepsis (LOS) [OR 1.71; 95% CI 1.34-2.19], severe intraventricular hemorrhage (IVH) [OR 4.64; 95% CI 3.51-6.14], patent ductus arteriosus (PDA) [OR 1.32; 95% 1.06-1.64], and mechanical ventilation (MV) [OR 2.03; 95% CI 1.54-2.67].
Conclusion: In surviving VLBW infants at discharge, a higher probability of PVL was associated with the presence of BPD, NEC, LOS, severe IVH, and PDA and the use of MV.

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright (c) 2025 Revista Chilena de Pediatría