Abstract
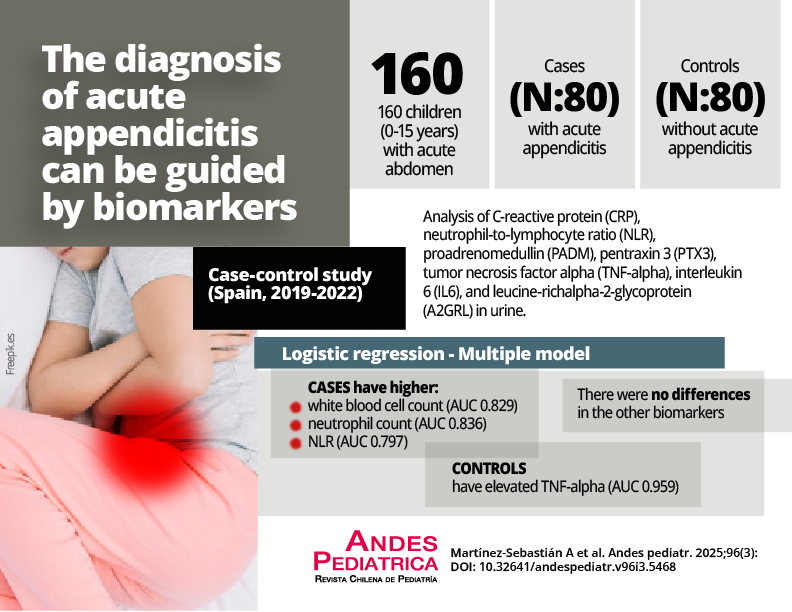
Acute appendicitis is a surgical emergency in pediatrics. An accurate diagnosis, based on new biomarkers, could reduce associated complications.
Objective: to assess the usefulness of blood and urine biomarkers in the diagnosis of acute appendicitis in pediatrics.
Patients and Method: Prospective, analytical, observational case-control study, conducted in a single center between 2019-2022. The study population consisted of 160 children aged between 0 and 15 years, divided into two groups (80 children with acute appendicitis and 80 without it), who consulted due to abdominal pain suggestive of acute abdomen, evaluated with biochemical markers and ultrasound for diagnosis. For evaluation, blood markers included C-reactive protein (CRP), neutrophil-lymphocyte ratio (NLR), proadrenomedullin (proADM), pentraxin 3 (PTX3), tumor necrosis factor alpha (TNF-alpha), and interleukin 6 (IL6) and the urine marker leucine-rich alpha-2-glycoprotein (LRG). Simple binary logistic regression models were estimated to study their association with the variables analyzed, estimation of a multiple model with a stepwise entry method, and subsequent obtaining of adjusted ORs and construction of ROC curves. We considered a p < 0.05 as significant.
Results: Compared with controls, leukocyte count (AUC 0.829), neutrophils (AUC 0.836), and NLR (AUC 0.797) were significantly higher in the appendicitis group (p < 0.001), while the TNF-alpha elevation (AUC 0.959) reduced the prediction of appendicitis, without differences in the other biomarkers analyzed.
Conclusions: The values of leukocytes, neutrophils, NLR, and TNF-alpha are those that best discriminate acute appendicitis from other etiologies of abdominal pain.

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright (c) 2025 Revista Chilena de Pediatría