Abstract
Sickle cell disease (SCD) is a genetic hemoglobinopathy defined by the presence of sickle hemoglobin (HbS) in erythrocytes. The migration phenomenon has transformed SCD into an emerging disease in countries where it was previously unknown.
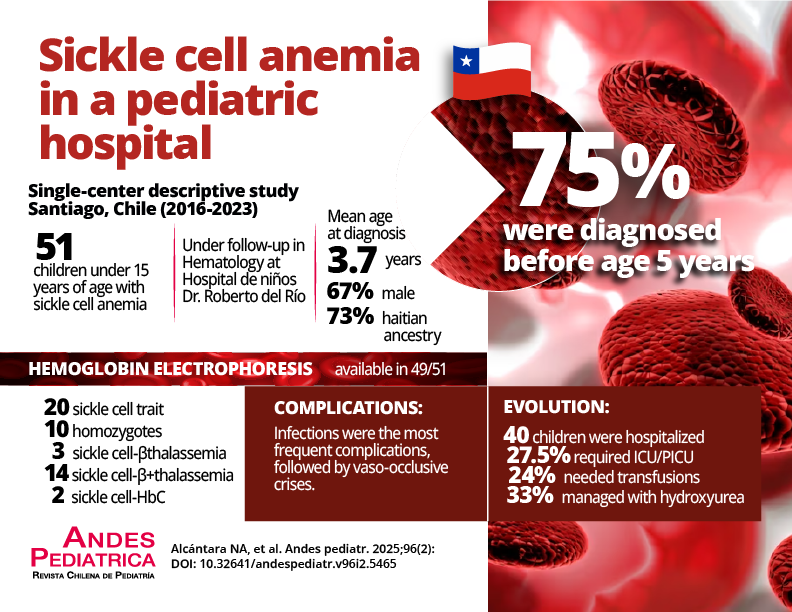
Objective: To describe the clinical and laboratory characteristics of patients with SCD diagnosed and under follow-up in a hospital in Santiago, Chile.
Patients and Method: Retrospective study of clinical and laboratory characteristics of 51 patients under 15 years of age with SCD, diagnosed and under follow-up at the Hospital Roberto del Rio (HRR) in Santiago, Chile, from March 2016 to December 2023. Epidemiological data, clinical manifestations, complications, analytical results, and treatments received were collected.
Results: The mean age was 3.7 years (75% diagnosed before age 5 years). 67% of patients were male. The most common ancestry was Haitian (73%), followed by Venezuelan (14%) and Colombian (8%). The most frequent finding was anemia (mean hemoglobin 10.3 gr/dL). Hemoglobin electrophoresis results were available in 49/51 patients (20/49 Sickle cell trait, 10/49 Homozygous, 3/49 Sickle cell-β-thalassemia, 14/49 Sickle cell-β+thalassemia, and 2/49 HbSC. Infections were the most frequent complications, followed by vaso-occlusive crises. Forty children were hospitalized and 27.5% required IMCU/PICU admission. 24% of patients needed transfusions and 33% were treated with hydroxyurea.
Conclusions: The study reproduces what is described in the medical literature. With diagnosis, early preventive treatment, and good medical care, morbidity can be minimized. Due to the increasing incidence of SCD, genetic counseling and the establishment of therapeutic guidelines are recommended.

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright (c) 2025 Revista Chilena de Pediatría